A complete guide to Sydney's North Shore birthing options.
You’ve just discovered you are pregnant. You’re feeling a flurry of emotions that might include joy, anxiety, excitement, or worry. You may have seen your GP to have your pregnancy confirmed, and just as you are trying to get your head around the fact you’re growing a new life inside your body, you have to make some decisions about your care.
The birth of your baby may feel like a long way off, but the decisions you make now can have a huge impact on your experience of pregnancy, labour, birth, and the postpartum period.
It can feel overwhelming, and it’s often easiest and most comfortable to do what friends or family members have done. To choose the route they did because if they’re familiar with it, then it must be okay.
But this is when it really pays to do your research. Through sickness, tiredness, the feeling like you’ve got the worst hangover since your 21st birthday party without the fun night beforehand, it pays to understand your options.
“A good birth has to be curated. It doesn’t just happen. It’s your responsibility to put things in place to optimise your chances that the birth you have will be the one you want.”
As a birth and postpartum doula, I support mums-to-be on the North Shore in Sydney, and I’ve put together a comprehensive guide on your choices when it comes to giving birth in our local area. It will help you understand what's available and make an informed choice that aligns with your preferences and needs.
*Disclaimer: I’ve spent days researching this information and it is true and correct to the best of my knowledge, however this guide should be used to support your own research.
Understanding Models of Care
What’s a model of care you ask? It’s a framework that forms the basis of maternity care. Not all models of care involve the same things, so knowing what each one typically includes, the benefits, potential risks and considerations, and typical cost, can help you decide what’s right for you.
Remember, each hospital, facility, or professional service provider’s model of care will differ slightly and you will need to understand how this looks directly from them. The following is a general guide only.
Standard midwifery-led care or midwifery clinics
What it looks like: Standard midwifery-led care or clinics place midwives as your primary caregivers throughout pregnancy, labour, and birth. You'll see a team of midwives (usually 6-8 different midwives) for your antenatal appointments, though you may not know which midwife will be present during your labour. Appointments are typically scheduled every 4-6 weeks until 28 weeks, then every 2 weeks until 36 weeks, and weekly thereafter. Expect around 7-10 appointments in total for a low-risk pregnancy. If complications arise, care is transferred to an obstetric team.
Benefits:
Evidence-based care focused on physiological birth processes
Lower rates of medical interventions compared to obstetric-led care
Emphasis on natural pain management techniques
Holistic approach considering emotional and social wellbeing
Cost-effective (free in public system)
Midwives are experts in physiological birth and can identify when medical input is needed
A stronger focus on breastfeeding support and postnatal care.
Risks and Considerations:
Less continuity of care - you may not know your labour midwife
May have longer wait times for appointments in busy public systems
Limited ability to accommodate specific requests or preferences
Less frequent monitoring compared to obstetric care.
Cost: Most of the cost of care is bulk-billed for Australian residents with Medicare-billed for Australian residents with Medicare
Midwifery Group Practice (MGP) for low-risk pregnancies
What it looks like: Midwifery Group Practice (MGP), sometimes known as 'Caseload Midwifery', is the work unit of caseload midwives enabling women to be cared for by the same midwife (primary midwife) supported by a small group of midwives throughout their pregnancy. Most MGPs will include around 4 midwives, each with a caseload of women to whom they provide continuity of care. The midwives in the Group provide back up to one another as needed, to maximise the likelihood that you’ll know the midwife who provides your care.
You'll be assigned a primary midwife who will be your main caregiver throughout your pregnancy journey. This midwife will care for you through your pregnancy, through your birth and at home for 10 days - 2 weeks after your baby is born. While you'll usually see your primary midwife, you'll also meet the other 3-4 midwives in the group during your pregnancy, so there's always a familiar face available when you go into labour. If complications develop requiring specialist care, you may need to transfer to obstetric-led care.
Benefits:
Continuity of care and carer is known to provide many benefits in terms of the health outcomes of mothers and babies and the levels of satisfaction of care for both consumers and care providers.
Women can form a relationship with a known midwife, improving both maternal and midwife satisfaction.
Higher rates of standard vaginal birth - In 2023 RHW MGP had a 67% normal vaginal birth rate, compared with the national average of 50.7%
Women are less likely to experience unnecessary intervention. Babies are more likely to be born healthy
24/7 on-call support from your known midwifery team
Active labour, physiological birth, breastfeeding and early discharge home from the Birthing Unit are a focus
Comprehensive postnatal support at home for up to 2 weeks
More personalised care with longer appointment times
Strong emphasis on building trusting relationships
Risks and Considerations:
Limited availability - MGP programs often have waiting lists due to high demand
Only suitable for low-risk pregnancies
Your primary midwife may occasionally be unavailable (though backup midwives from your group provide coverage).
Cost: Most of the cost of care is bulk-billed for Australian residents with Medicare
Maternity Antenatal Postnatal Service (MAPS)
MAPS (Maternity Antenatal Postnatal Service) is a public hospital continuity-of-care model that involves a small team of MAPS midwives. You receive antenatal care with a known midwife (and obstetricians if required) at the hospital. You give birth to your baby in the hospital’s birth unit where the midwives on duty will look after you during labour and birth. After you are discharged from the hospital, your known midwife (or the midwife team) provide your postnatal support.
This model provides comprehensive antenatal care that includes longer appointment times with a focus on pregnancy education and birth preparation tailored to your needs. After you’ve had your baby, you’ll receive extended postnatal support and home visits that provide breastfeeding support and guidance as well as family planning and contraception advice.
Benefits:
Continuity of antenatal and postnatal care with a known midwife team
MAPS midwives are specially trained in low risk pregnancy and postnatal care and can provide the majority of your care
Lower cost than private midwifery care - free as a public hospital service
Enhanced postnatal support
Personalised care with longer appointment times during pregnancy
Strong focus on education and preparation for parenthood
If medical consultation or referral is needed, the team can organise this while continuing to provide your care alongside doctors
Ideal for women wanting continuity but comfortable with hospital birth midwives
Risks and Considerations:
Different midwife attends your birth than the one providing antenatal and postnatal care
Suitable for low-risk pregnancies without complications requiring specialist care
Birth experience similar to standard hospital care rather than midwifery group practice
Cost: Most of the cost of care is bulk-billed for Australian residents with Medicare.
GP Shared Care
What it looks like: GP shared care is a collaborative model where your family doctor provides most of your antenatal care, working in partnership with the hospital's midwifery team. You'll have regular appointments with your GP (similar schedule to midwifery care), with specific appointments at the hospital at key times - typically around 12-16 weeks for booking, 36 weeks for birth planning, and any time complications arise. Your GP conducts routine checks, orders tests, and monitors your pregnancy, while the hospital team manages your labour and birth.
Benefits:
Continuity with a doctor you know and trust
Convenient local appointments with your regular GP
Your GP understands your medical history and family context
Often easier to get timely appointments
If complications develop, you're referred back to hospital care
Good integration between pregnancy care and ongoing family health
Cost-effective for routine, low-risk pregnancies
GP can continue postnatal care and baby's early health checks
Risks and Considerations:
Your GP won't be present during labour - hospital midwives manage birth
Potential for communication gaps between GP and hospital team
GPs vary in their obstetric experience and comfort level
May miss subtle complications that specialist-trained midwives or obstetricians would catch
Less specialised pregnancy and birth education compared to midwifery-led care
Cost: Most of the cost of care is bulk-billed for Australian residents with Medicare
Public Obstetric Care or Clinic for High-Risk Pregnancies
What it looks like: This model involves care by specialist obstetricians (doctors who specialise in pregnancy, labour, and birth) within the public hospital system. You're referred to this care if you have medical conditions, pregnancy complications, or risk factors that require specialist monitoring. Appointments are more frequent and longer, typically involving detailed ultrasounds, specialised tests, and care planning. A multidisciplinary team may include maternal-fetal medicine specialists, endocrinologists, cardiologists, or other specialists as needed.
Benefits:
Expert management of complex medical conditions during pregnancy
Access to advanced diagnostic tools and monitoring equipment
Immediate access to emergency interventions if needed
Coordinated care with other medical specialists
Higher staffing ratios and more intensive monitoring during labour
Access to neonatal intensive care if baby needs special care
Evidence-based management of high-risk conditions
Risks and Considerations:
Higher rates of medical interventions, including caesarean sections
Less emphasis on natural birth approaches
More medicalised approach may increase anxiety for some women
Less continuity - you may see different specialists at different appointments
Longer wait times and busier clinic environments
May feel less personal than midwifery-led care
Higher likelihood of induction of labour or early delivery
Conditions typically requiring specialist obstetric care include:
Diabetes (pre-existing or gestational)
High blood pressure or pre-eclampsia
Previous pregnancy complications
Multiple pregnancies (twins, triplets)
Placental problems
Fetal growth restrictions
Maternal heart conditions
Previous caesarean sections (in some cases)
Cost: Most of the cost of care is bulk-billed for Australian residents with Medicare
Private Obstetrician Care
Private obstetric care involves choosing your own specialist obstetrician who will manage your pregnancy, birth, and initial postnatal care.
What it looks like: You select an obstetrician based on recommendations, hospital privileges, or personal preference. Your obstetrician will be your primary caregiver throughout pregnancy and will personally deliver your baby (or arrange coverage with a trusted colleague). Appointments are typically monthly until 28 weeks, fortnightly until 36 weeks, then weekly. Consultations are usually 15-30 minutes and include physical examinations, ultrasounds, discussions about your pregnancy progress, and planning for birth.
Benefits:
Continuity of care - you know exactly who will deliver your baby
Longer consultation times allow for detailed discussions and questions
Flexible scheduling often with same-day or urgent appointments available
Choice of private hospital with enhanced facilities and amenities
Ability to plan timing of birth (including elective caesarean scheduling)
Direct mobile phone access to your obstetrician for urgent concerns
Personalised care tailored to your specific needs and preferences
Expert management of any complications that arise
Comprehensive postnatal follow-up typically for 6 weeks
Risks and Considerations:
Higher intervention rates compared to public care - studies show private patients have significantly higher rates of caesarean sections, instrumental deliveries, and other interventions
Caesarean rates in private care can be 1.6 times higher than in public care for low-risk women
More medicalised approach may not suit women wanting natural birth experiences
Significant financial commitment even with private health insurance
May have less emphasis on midwifery support and natural pain management
Potential for unnecessary interventions due to scheduling pressures or risk-averse practices
Limited availability of some obstetricians due to high demand
Approximate Costs:
Obstetrician fees: $3,000-$8,000+ (gap fees after insurance/Medicare rebates)
Hospital accommodation and theatre fees covered by private health insurance
Anaesthetist fees (if epidural or caesarean required): $500-$2,000+ gap
Paediatrician fees for baby checks: $300-$800+ gap
Additional specialist fees if complications arise
Additional costs for premium room upgrades, extended stays, or additional services
Total out-of-pocket costs typically $5,000-$15,000+ depending on complications and services used.
Prerequisites:
Private health insurance with obstetric cover (12-month waiting period applies)
Financial capacity to cover gap fees
Must book early as popular obstetricians fill up quickly
Private Obstetrician in a public hospital
This model of care combines elements of private obstetric care with the public hospital system. Some obstetricians work in public hospitals while also maintaining private practices. In this arrangement, you choose and pay a private obstetrician who has privileges to work within a public hospital. You receive private obstetric care throughout your pregnancy in their private rooms, but give birth in the public hospital.
What it looks like: You see your chosen obstetrician for all antenatal appointments at their private consulting rooms, following the typical private care schedule. When you go into labour, you attend the public hospital where your obstetrician has arrangements. You'll be admitted as a public patient but receive care from your private obstetrician as well as the midwives on duty in the birth and maternity wards.
Benefits:
Continuity of care with your chosen obstetrician throughout pregnancy and birth
Significantly lower costs compared to private hospital care
No requirement for private health insurance with obstetric cover
Access to public hospital facilities including comprehensive emergency services
Your obstetrician personally attends your birth
Longer consultation times during pregnancy typical of private care
Access to advanced public hospital facilities and specialist services
Lower overall intervention rates compared to private hospitals.
Risks and Considerations:
Limited availability - not all obstetricians offer this service
Your obstetrician may not be available 24/7 (backup arrangements with colleagues)
Less choice in birth environment and amenities
May have hospital policies that limit some preferences
Limited partner accommodation compared to private hospitals
Approximate Costs:
Obstetrician fees: $3,000-$6,000+ (often lower than full private hospital care)
No hospital accommodation fees - covered as public patient
Medicare rebates may be available for obstetric consultations
May still require gap fees for anaesthetist services if epidural or caesarean needed
Total out-of-pocket costs typically $3,000-$8,000
Private Midwife Care or Privately Practising Midwives (PPM)
Private midwives offer personalised, woman-centred care throughout pregnancy, birth, and the postnatal period. They can attend births at home, in birth centres, or sometimes in hospitals depending on their credentials and hospital privileges.
What it looks like: You choose a private midwife who becomes your primary caregiver throughout your maternity journey. Appointments are typically longer (45-60 minutes) and held in the midwife's clinic, your home, or via telehealth. Your midwife provides comprehensive care including antenatal education, birth preparation, labour support, and extensive postnatal care. Many private midwives work in small group practices (2-4 midwives) to provide backup coverage.
Benefits:
True continuity of care - you know exactly who will attend your birth
Personalised, unhurried care with extensive time for questions and education
Holistic approach considering physical, emotional, and social wellbeing
Strong advocacy for your birth preferences and informed consent
Comprehensive birth preparation and education tailored to your needs
24/7 availability during late pregnancy and labour
Extensive postnatal support including home visits for several weeks
Lower intervention rates compared to obstetric-led care
Flexible care arrangements that can adapt to your changing needs
Strong focus on natural birth approaches and normal physiology
Immediate and ongoing breastfeeding support
Family-centred care that includes your partner and other children
Risks and Considerations:
Limited ability to manage high-risk pregnancies or complications requiring specialist intervention
If complications arise requiring obstetric care, you may need to transfer care models
Not covered by Medicare for all services, requiring significant out-of-pocket expenses
Limited availability - many private midwives have waiting lists
Varies significantly in experience and qualifications between practitioners
Some don't have hospital privileges, limiting birth location options
Less immediate access to emergency interventions compared to hospital settings
Approximate cost:
Varies from midwife to midwife but complete midwifery care can range from $3,000-$7,000 depending on services included.
Antenatal care only: $1,500-$3,000
Postnatal care packages: $800-$2,000
Australian residents with Medicare can expect rebates for some midwifery services
Private health insurance may provide ancillary rebates
Additional costs may apply for birth pool rental, supplies, or travel
Australian residents with Medicare and Private health Insurance out of pocket costs will vary depending on individual level of coverage and Health fund.
Now you’re aware of the different models of care typically available, it’s time to look at the locations and facilities you may want to consider. I have done my best to research and list the most well-known options in the North Shore. However, this should form part of your overall research and there may be other options available that I’m unaware of and are not listed here.
Public Hospitals in the North Shore
Hornsby Ku-ring-gai Hospital
Level 2, Building 50
Hornsby Ku-ring-gai Hospital
Palmerston Rd, Hornsby, 2077, NSW
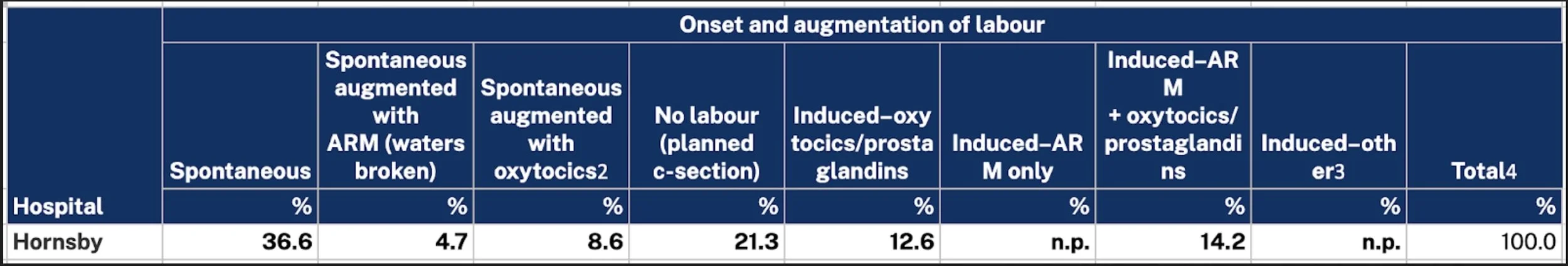
Hornsby Ku-ring-gai Hospital serves the Upper North Shore area. The hospital provides care for approximately 1,200 births per year and is part of the Northern Sydney Local Health District. It is a small, intimate public hospital compared to Royal North Shore Hospital (the other public hospital in our area). The facility has 25 dedicated maternity beds and offers comprehensive maternity services. It has experienced midwifery and obstetric teams who provide care for low-risk and high-risk pregnancies.
Hornsby Hospital a glance
Comprehensive antenatal care
Labour and birth support across all care models
Water birth facilities for eligible women
Postnatal care and breastfeeding support
Access to social work and support services
Transfer arrangements to Royal North Shore Hospital if needed
Pregnancy, birth and parenting education classes
Models of Care available
Midwifery Group Practice (MGP)
Midwifery Care/Clinics
Maternity Antenatal Postnatal Service (MAPS)
GP Shared Care
Public Obstetric Clinic
Private Obstetrician
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
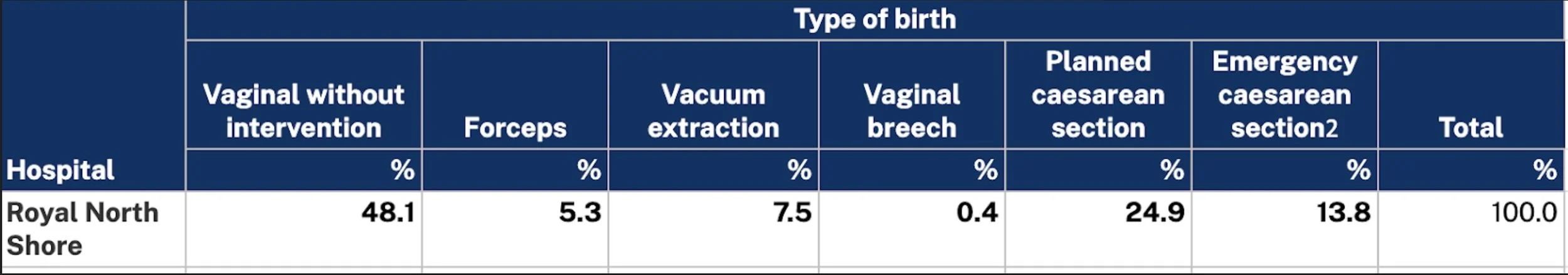
Royal North Shore Hospital (RNS)
Women's Health Ambulatory Care
Level 3 - Clinical Services Building
Royal North Shore Hospital
1 Westbourne Street
St Leonards, 2065
Royal North Shore Hospital is the major public teaching hospital serving the North Shore area. The hospital provides care for approximately 2,000 births per year and is part of the Northern Sydney Local Health District. The hospital has 9 birthing rooms featuring mats, birth balls, bean bags, and birthing pools, All but one birthing room is equipped for water births. The maternity unit has 40 maternity beds in single and shared rooms, all with ensuites. It has a Neonatal Intensive Care Unit with 32 cots.
Royal North Shore a glance
As a level 6 maternity capability hospital, RNS is highly equipped to provide a comprehensive array of services.
Extensive early pregnancy support
Specialist care for high-risk pregnancies
Labour and birth support across all care models
Water birth facilities for eligible women
Postnatal care and breastfeeding support
Access to social work and support services
Pregnancy, birth and parenting education classes
Models of Care available
Midwifery Group Practice (MGP)
Midwifery Care/Clinics
Maternity Antenatal Postnatal Service (MAPS)
GP Shared Care
Public Obstetric Clinic
Private Obstetrician
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
Northern Beaches Hospital
105 Frenchs Forest Rd W,
Frenchs Forest , NSW 2086
Northern Beaches Hospital (NBH) is a hospital that serves both public and private patients and provides care for approximately 1,600 births per year. The hospital has 10 birthing suites, three of which have birthing pools. If you have private health insurance, you can choose your obstetrician and access the facilities of a private experience. If you book in as a public patient, you can choose from the hospital’s range of care models including midwifery-led care and GP shared care. They also offer the private experience for mums without private health insurance who wish to pay to stay.
North Beaches Hospital at a glance
Private and public options available
Pregnancy and birth education classes
Water birth facilities for eligible women
Experienced midwives who can support holistic birth such as hypnobirthing
Postnatal care for up to fourteen days in some models of care
Models of Care available:
Private Obstetrician
Midwifery Group Practice (MGP) for low-risk pregnancies
Standard midwifery-led care
GP shared care
Hybrid public-private packages
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
Private Hospitals in the North Shore
North Shore Private Hospital
3 Westbourne St,
St Leonards, NSW 2065
North Shore Private has a collaborative team of obstetricians, paediatricians, midwives, social workers and lactation experts that support you through your pregnancy and birth. The hospital has 7 birthing suites and provides care for around 2,500 births per year. It is co-located with the public Royal North Shore hospital providing access to tertiary care facilities, including the NICU if needed. You have a private room and your partner can usually stay overnight. You can choose your Obstetrician who will provide your ongoing care. If you do not have private health insurance, the hospital offers a pay and stay option.
North Shore Private at a glance
Luxury birthing suites with hotel-style amenities and comfort
Comprehensive maternity and postnatal education programs
No water birth facilities
Access to extra support up to when your baby is 12 months old
Access to emotional wellbeing support from a Gidget Foundation Psychologist
Models of Care available:
Private Obstetrician
Pay to Stay
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
Mater Hospital North Sydney
25 Rocklands Rd,
Wollstonecraft, NSW 2065
The Mater offers integrated collaborative care combining obstetricians, midwives, and support staff with Catholic healthcare values. The hospital combines medical expertise with holistic care principles, often incorporating spiritual and emotional support alongside clinical care. It provides care for around 2,000 births per year and has six dedicated birthing suites, including three that are equipped with a freestanding bath for water immersion during labor. you have a private room and your partner can usually stay overnight. You can choose your Obstetrician who will provide your ongoing care. If you do not have private health insurance, the hospital offers a pay to stay option.
Mater Hospital at a glance
Collaborative care model combining medical and midwifery expertise
Childbirth, breastfeeding, parenting and postnatal education
No water birth facilities
On-site paediatric services and Level 4 Special Care Unit (SCU) for immediate baby care if needed
Access to additional support services including social work and pastoral care
Models of Care available:
Private Obstetrician
Pay to Stay
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
Sydney Adventist Hospital (The San)
185 Fox Valley Road,
Wahroonga, NSW 2076
Sydney Adventist Hospital is a private hospital that operates as a not-for-profit organisation under the Seventh-day Adventist Church. A multidisciplinary team of obstetricians, midwives, mothercraft nurses and paediatricians work together to provide care for around 1,700 babies per year. The San’s maternity unit has nine birthing suites, two of which are equipped for water births. There are 40 private rooms that include ensuites, breastfeeding chairs, and purpose-built baths. Some rooms have double beds while others have day beds for partners or support persons to use overnight. You can choose your Obstetrician who will provide your ongoing care.
Sydney Adventist Hospital at a glance
Comprehensive maternity and postnatal education programs
Access to on-site special care nursery with transfer to the Royal North Shore Hospital, The Children's Hospital at Westmead NICU if required.
Spiritual care and pastoral services available
Skilled team of educators, lactation consultants and highly experienced nursing staff
Models of Care available:
Private Obstetrician
Pay to stay
Intervention rates and other statistics
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
Source: NSW Mothers & Babies Report 2023
Public & Private Hospital birth statistics.
So you can compare intervention rates and other statistics more easily, I’ve compiled them into the following tables. You can view the original spreadsheet here.
Onset and augmentation of labour
Type of birth
Pain relief
Perineal status
n.p. = not published
Home Birth Options.
Home birth is a growing option for low-risk pregnancies that is supported by substantial research evidence. Currently, 97% of births in Australia occur in hospitals.
Home birth involves giving birth in your own home with the support of registered midwives experienced in home birth care. Your midwife will visit you throughout pregnancy for antenatal appointments, be on-call for labour, attend you throughout labour and birth at home, and provide postnatal care for several weeks. Your home is prepared with birth supplies, and you create the environment you want - dim lighting, your own music, familiar surroundings, and unlimited support people.
Currently, none of the hospitals in the North Shore offer a Publicly Funded Home Birth (PFHB). You can find a list of the hospitals that are part of the current consortium here.
If you would like to explore homebirth, you will need to hire a Privately Practising Midwife (PPM). You should speak to several midwives to determine whether a homebirth with a PPM in attendance is an option for you, as they all have different acceptance criteria.
PPMs & Homebirthing Centres in the North Shore
Serving the Northern Beaches and surrounding suburbs
Offering woman-centred/family-centred holistic midwifery care, they offer home-birthing, continuity of care, childbirth education, perinatal support and infant massage, to assist you and your family through this ever-changing chapter in life.
Serving North Sydney
Offering pregnancy, labour and birth, and postnatal support through a practice that is grounded in the belief that childbirth is a powerful and transformative experience.
Serving Greater Sydney
Blooming Hearts provides women and their families in the Greater Sydney area with private midwifery services.
ibirth
Serving Northern Beaches, Upper North Shore/ Hornsby Shire & Sydney
Forming relationships with women and their families and providing a continuation care model enables trust, communication, respect, education, support and care.
Find more privately practising midwives at Homebirth NSW
Choosing a Private Midwife:
Verify registration with Australian Health Practitioner Regulation Agency (AHPRA)
Check professional indemnity insurance coverage
Ask about their experience, philosophy, and approach to care
Understand their backup arrangements and transfer protocols
Confirm their birth attendance locations and hospital privileges
Discuss their collaboration with other healthcare providers
Review their emergency procedures and equipment.
Other Support Options.
Doula Support
While not a care provider, doulas offer continuous emotional and physical support during labour and birth. They work alongside your chosen model of care to enhance your birth experience.
What Doulas Provide:
Emotional support and advocacy
Physical comfort measures
Birth preparation and education
Support for partners
Immediate postnatal assistance
Costs: Varies from doula to doula but expect to pay between $2,000-$4,000
Learn more about my birth and postpartum services.
Private Midwife Home Visits
Specialist service that gives you extra confidence and care in the comfort of your home. They offer support and advice for anything and everything to do with pregnancy, birth and baby. These midwives don’t replace the care from your usual care team, but are available to supplement it with valuable care when you need it.
Costs:
Home visit with a Medicare card: $250 travel fee applies (the appointment itself is bulk-billed)
Home visit without a Medicare card: $400 ($150 appointment fee and $250 travel fee)
Telehealth via phone or Zoom with a medicare card: Free (the appointment is bulk-billed).
Making your decision.
There’s a lot to think about when choosing a facility and model of care. The below considerations can help you as you make your decision.
Your birth preferences: Do you prefer physiological birth approaches, or are you open to medical interventions? Different care models have varying intervention rates.
Continuity of care: How important is it to know who will be caring for you during labour? Or is trusted support more crucial for you during pregnancy and in the weeks after you’ve had your baby.
Your risk level: If you have pre-existing medical conditions, you may require specialist obstetric care, while low-risk pregnancies have more options available.
Budget: Consider both upfront costs and potential gap fees. Public options are pretty much totally free, while private care involves significant costs, even with private health insurance.
Location: Consider travel time during labour and postnatal convenience for follow-up care.
Support network: How important are visiting arrangements, partner accommodation, and family support needs for you?
Planning ahead
Start researching your options early in pregnancy, ideally by 12-16 weeks, to ensure you can secure your preferred care provider and have time to build a relationship with them before your birth.
Remember, your birthing experience is personal, and the best option is the one that feels right for you and your family. Take time to research, ask questions, and trust your instincts when making this important decision.
This guide provides general information about some of the birthing options on Sydney's North Shore. It should form part of your research, but it is advised you undertake additional research as well. Always consult with a healthcare professional for personalised advice based on your individual circumstances and medical history.
Contact Kelly
If you have any questions or would like more info, I’d love to hear from you. Get in touch by clicking the button below and completing the contact form.
About Kelly Allen
My name is Kelly, and I’m a certified birth and postpartum doula who trained at the Doula Training Academy. I service women and birthing people in the North Shore of Sydney, helping you enter and emerge from birth and the fourth trimester feeling physically and emotionally well.